Healthcare shortage in rural India – How’s it being handled ?
Rural India is starved for doctors and health care facilities and its a big problem!
The scenario has multiple angles to it where – states like Karnataka are pushing for a compulsory two year bond among MBBS students, rural healthcare centres lack basic amenitites, MBBS students validate their side of the argument by saying a rural posting could lead to patients relatives attacking them and there would be no protection against this, practicing doctors are divided in their opinions with some saying that putting a fresh MBBS doctor in a rural setting is equivalent to placing a fresh engineering graduate in charge of the country’s space program. Others say that it is a medical students duty to take up rural services simply because it is part of a ‘doctor’s duty’.So which angle is correct? Let’s take a look at the factors
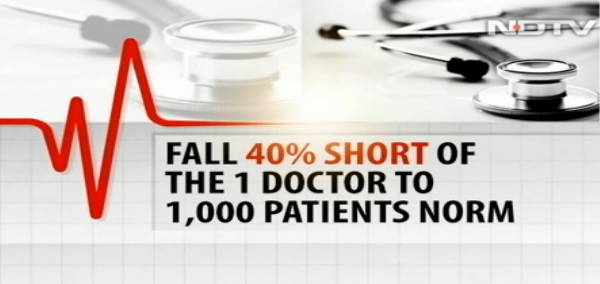
The Shortage – India as a whole has the following statistics that reflect a low number of doctors overall. Based on National Health Mission Report Data there is-
– 82% shortage of surgeons, physicians and paediatricians.
– In 2013 the country had 5,805 specialists whereas in 2014 it dropped by 1,714 to 4,091 specialists
– WHO norms recommend 1 doctor for every 1,000 patients. India falls 40% short of this figure
– For a 120 crore population there are only 2 lakh surgeons and less than 50,000 Pediatricians

Now based on the above shortage when we look at rural India we see that 70% of the country’s population is in rural India but only 33% of the country’s doctors cover the rural areas. To address this shortage, a 3-year BSc Community Health program was initiated in 2007 and it would “train practitioners in conducting normal deliveries, pre-natal and anti-natal care and vaccination as well as in treating diarrhoea, pneumonia, tuberculosis, fevers and skin infections”. They would, however, not be qualified to treat or diagnose more serious diseases. After completing the course and six months of internship, they would be under an obligation to serve in rural areas for at least five years. Thereafter, could undertake a two-year bridge course and get an MBBS equivalent qualification. Only, the course never saw the light of day.
The 3 + 2 Government Formula
On Sep 2, 2015 the Delhi high court, heard a petition filed by advocate Prashant Bhushan, pulled up the health ministry and the MCI for failing to implement the course. The MCI however went on to say – a ‘science graduate’ wouldn’t have the adequate knowledge to substitute a regular doctor, to allow a BSc Community Health graduate to practice as a doctor the Indian Medical Council Act would have to be amended. Currently, such a graduate can only work under the supervision of an MBBS doctor. The MCI has also said that its up to each state to decide to what extent they want to put this program into effect.These individuals could also take a 2 year add on course that could then qualify them as an MBBS.
Revive the Course!
While the MCI isn’t too keen to implement it, supporters of the BSc course say it would help- reduce the shortfall of doctors in rural areas, help identify and treat basic disesases and only send the complicated cases to healthcare centres preventing overflowing OP wards and looking at a rural setup’s basic needs alone a practitioner who can diagnose and treat basic ailments is very necessary.
Half baked doctors, leads to Quacks?
The question then arises would such a practice lead to quackery? Mihir Banerjee of People for Better Treatment, an NGO that campaigns against medical malpractice says “Just because it’s rural does not mean a place deserves any less than a qualified doctor.” AV Jayakrishnan, secretary of the Indian Medical Association’s Kerala chapter agrees. “MBBS is the basic course for all medical doctors. Any further dilution can be detrimental to healthcare. Less qualified doctors won’t be able to diagnose complex life-threatening diseases. There should be no discrimination against rural areas in this respect.” Jayakrishnan claims the course is part of the government’s plan to certify homeopathic and ayurvedic doctors as qualified medical practitioners.
The West Bengal Model
In light of the two sides above, the state of Bengal has an interesting scenario where in Dighul village in Birbhum district, Santosh Ghosh is ‘daktarbabu’. Just class 10 pass. He has been giving injections, medicines and even stitching small wounds for the last 25 years. For the villagers, he is god. The local government health centre is 2 km away but a doctor visits for only a few hours a day. For the villagers, Mr Ghosh is always there at his home cum chamber.Ashok Kundu has a BSc degree and a lab technician’s diploma. But, like Mr Ghosh, no MBBS.
Agree or disagree, these people are helping meet the problem at its root and providing a service that otherwise people didn’t have access to.
When asked about the word ‘quack’ Mr. Kundu angrily said, “Quack means magic in Bengali. But we don’t do magic. We treat people, help them get to a hospital in a crisis. We are not quacks or magicians! Mr. Kundu understands the apprehension behind him being called a doctor and quickly adds on,”The people call us ‘doctor’, You can call us rural health care providers. If government gives us some recognition, some training, we can help in giving health care in rural areas.” They are willing to help with rural healthcare and there are many such practitioners across villages in Bengal doing the same.
At present, these practitioners are being trained for a 9 month duration by the Liver Foundation (NGO) with government support. The NGO is confident that the training method can be standardized with further government support. The NGO is already in talks with state governments of states like Uttar Pradesh, Rajasthan and MP to setup similar programs and insert these individuals on the fringes of the healthcare system.
IMA’s Argument:
The IMA has two points to counter the NGO and such practitioners. First, it suggests an increase in the number of MBBS seats rather than putting up a diluted course. Secondly, they strongly oppose such practitioners and Dr Santanu Sen, secretary of IMA Bengal chapter, said: “IMA is promoting the anti-quackery movement nationwide. How do you regulate or enlist quacks? Yes, they should be enlisted by the local administration so they can’t harm any person.”
MBBS Students
The question and issue however remains of medical students who look for escapes from rural services even as state governments are starting to make it compulsory and pushing it as a “student’s duty” and that the country’s interest always trumps an individual’s needs or desires. Students presents a counter argument and state that there have been cases in rural areas where when a patient couldn’t be treated, relatives have come after and even killed doctors. In a time where attacks on doctors are on the rise, this too is a convincing argument!
Tailor Made Solution?
A tailor made solution to tackle this would be for individual state governments to create a program to incubate individual villages, build up healthcare infrastructure and rotate (even MBBS doctors) on a 6 month basis, provide a ticket based patient queuing system to prevent overflow or possible attacks on doctors and most definitely security. While this may seem too perfect, if done right and fine tuned as it goes; it is an achievable model. But until that time, while course certainly isn’t an ideal solution it would provide much-needed relief to some of the country’s most marginalised population. That’s reason enough to give it a try. With shortage in doctors, MBBS students uncomfortable with serving in rural areas and medical practitioners willing to ‘help’ such an initiative could be a good point to start as a foundation. Better some service than none at all?
Original Story – NDTV Special Feature and Catch News
Image Credits : Catch News
Enjoyed reading this news story? For MORE medical discussions,image cases, MCQs and cases download the DAILY ROUNDS app for FREE! at App Store or Play Store


In assam rural health practitioner now Community health officer doing good job… You can collect data from NRHM assam website..