
When COVID-19 Opens Up The Fault Lines In India’s Healthcare Infrastructure

With the number of coronavirus cases steadily rising even after the lock-down period, the healthcare infrastructure of the country has started to creak as major cities run out of resources. Ever since the arrival of the pandemic, India has been hearing the word ‘shortage’ from time to time. As the initial days witnessed a shortage of Personal Protective Equipment (PPE), today, the nation is facing a significant shortage of doctors, healthcare workers, hospital beds, and other medical equipment.
The country now has over 2,60,000 COVID-19 cases with major metros Mumbai and Delhi affected the worst. Reports from across the cities certainly indicate a healthcare system in distress as the shortage of healthcare workers and beds prompts hospitals to turn away patients seeking tests and treatment for COVID-19 and other ailments. With cases rising daily at an alarming rate fault lines in India’s health infrastructure are out in the open.
Running Out Of Resources
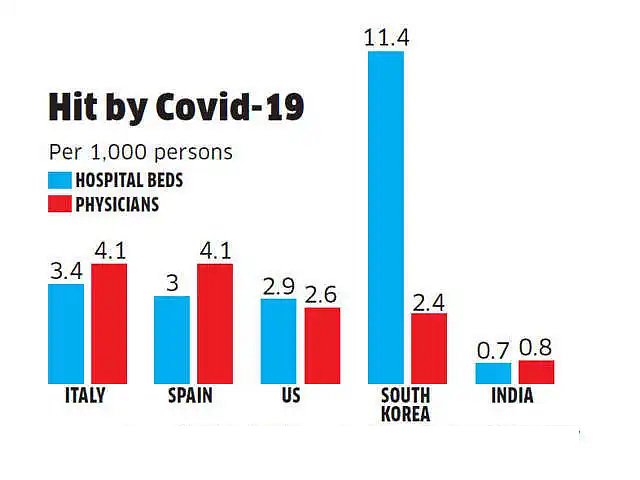
As per the data bank of the World Health Organization (WHO), India has only 0.7 hospital beds for every 1000 people in the country whereas, the global average stands at 2.7 beds per 1000 people. The ratios in some of the states are even more terrifying.
Maharashtra, one of the worst affected states in the country has surpassed China, the original coronavirus epicenter when it comes to the number of confirmed cases. According to the data provided by the National Health Profile (NHP) 2018, the state has a total of 711 public hospitals with 51,446 beds, a number that was inadequate even in a non-pandemic scenario. As per NHP, there is only one government hospital in Maharashtra for every 1,66,880 people.
Even though the Maharashtra government has asked the authorities to take charge of 80% of beds in private hospitals, complaints of patients unable to find beds are pouring in. According to the health department, there are 16,197 COVID-19 beds in Mumbai of which over 80% are occupied. Also, the latest data from BMC shows that 99 percent of the total intensive care unit (ICU) beds are full and 94 percent ventilators are occupied in public and private hospitals in Mumbai. The city has 1,094 ICU beds in public and private hospitals out of which 1,083 are full and out of 464 ventilators in public and private hospitals, 437 are already occupied.
Along with this, the shortage of front-line healthcare workers in the state is rubbing salt into the wound. Many hospitals across the state are currently running out of doctors and nurses. To overcome the crisis, Maharashtra had recently sought 50 specialist doctors and 100 nurses from Kerala. A drastic increase in the infection rate among healthcare workers has worsened the situation in the state.
Meanwhile, the national capital with 27,654 confirmed cases is already under the scanner of the Union Health Ministry for low testing, rising number of cases, and patients’ complaints. With cases increasing by around 1,000 every day, denial of treatment, especially in private hospitals, is rising in tandem.
Recently, Delhi’s Deputy Chief Minister Manish Sisodia said that the capital will have more than half a million COVID-19 cases and it does not have the hospital capacity to handle such an outbreak. He said the city will need 80,000 hospital beds to tackle the spike. Sisodia’s warning came as harrowing accounts of people struggling to get a hospital bed in New Delhi emerged, including some who said their loved ones died on the doorsteps of medical centers that refused to take them in.
Tamil Nadu, another COVID-19 hotspot in the country, logged around 1562 cases the previous day, taking the total case tally to 33,229. Following the surge in the number of cases, the state health department has ordered additional oxygen pipes and cylinders to be placed at out-patient clinics to ensure quick treatment of patients coming with hypoxia. The shortage of oxygen cylinders in Chennai is not an isolated case, many hospitals across the country are also facing similar issues.
The ‘Makeshift’ Plans

Setting up a hospital with all basic amenities within a fortnight is no longer a fairy tale. Makeshift hospitals have popped up across the globe to handle the surge of COVID-19 patients. India would require a large number of such makeshift hospitals, in addition to the existing ones, to handle the present crisis situation.
Number of COVID-19 cases is constantly increasing and at some point of time in the near future, apart from existing hospitals, a large number of temporary, makeshift hospitals will have to be created to accommodate COVID-19 patients requiring admission, medical care, and treatment.
The health ministry said to the Supreme Court in an affidavit
Meanwhile, the Mumbai Metropolitan Region Development Authority (MMRDA) has constructed a makeshift 1,000-bed mega-hospital in its efforts to tackle the coronavirus outbreak. In a similar move, the stadiums, along with other luxury hotels in the national capital will soon be transformed into healthcare facilities. In a bid to increase the country’s capacity for isolation facilities, the Indian railways has converted many of its sleeper class coaches into Covid isolation wards suitable to act as quarantine hubs. The railway coach quarantine wards are expected to meet any exigency as and when the government requires.
However, to create an optimum infrastructure to provide proper medical care to COVID-19 patients, the central government will also have to adequately address the human resource issue prevailing at the moment. Hence conserving and ensuring the well-being of the healthcare workforce has become the need of the hour to cater to the anticipated patient load in the hour of distress.
Healthcare infrastructure is not something that should come to the limelight during a pandemic or outbreak especially in a country like India with over 1.35 billion population. A long term action facilitating the overall development of healthcare infrastructure should become the priority of the nation. For this, a specially designed fiscal stimulus has to be funnelled into the public health sector. The healthcare workers at the forefront should be provided with proper infrastructural facilities and equipment so that they can do their part in the best possible way.
Remember, not even Shakespeare’s characters can play their roles in the absence of ‘stage’ and ‘props’!